Cataracts - InDepth
Highlights
Cataracts are a common age-related vision problem that involves clouding of the lens in the eye. Cataracts are responsible for about one half of the world's blindness. Developing countries bear the brunt of blindness caused by cataract, due to higher incidence, lower age at onset, and less access to eye care compared to developed countries. In the United States, about 24 million people age 40 and older have cataracts. The older a person gets, the greater the risk of developing cataracts. Women are more likely to develop cataracts than men.
In addition to age, other factors may increase the risk for cataract development. These include:
- Diabetes
- Smoking
- Overexposure to sunlight
- Certain medications, such as steroids
During the early stages, cataracts may have little effect on vision. Symptoms vary due to the type of cataract (nuclear, cortical, or posterior subcapsular.) Depending on the type and extent of the cataract, people may experience the following symptoms:
- Cloudy vision
- Double or blurry vision
- Glare and sensitivity to bright lights
- Impaired color vision
- Difficulty reading due to reduced black-white contrast
- Difficulty driving at night
Cataracts never go away on their own, but some stop progressing after a certain point. If cataracts continue to progress, they can cause blindness if left untreated. Fortunately, cataracts can almost always be successfully treated with surgery. Millions of cataract operations are performed each year in the United States, and there is a very low risk for complications. However, before opting for surgery, people need to consider on an individual basis how severely a cataract interferes with their quality of life. Cataract surgery is rarely an emergency, so people have time to consult with their doctors and carefully consider the risks and benefits of surgery.
Surgery involves removing the cataract and replacing the abnormal lens with a permanent implant called an intraocular lens (IOL). The operation is generally painless, takes less than 1 hour and is performed on an outpatient basis. Most people remain awake, but sedated, during the procedure. If you have cataracts in both eyes, doctors recommend waiting at least 1 to 2 weeks between surgeries.
Introduction
A cataract is an opacity, or clouding, of the lens of the eye.
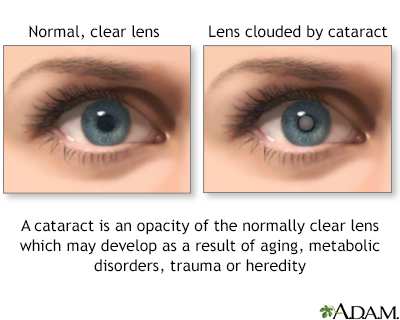
The lens is normally clear. If the lens becomes cloudy or is opacified, it is called a cataract.
The likelihood of developing cataracts increases with age. Cataracts typically develop in the following way:
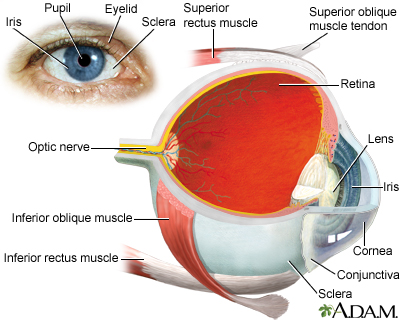
- The lens is an elliptical structure that sits behind the pupil and is normally transparent. The function of the lens is to focus light rays from objects in front of the eye, forming mirror images that are projected onto the retina (the light-sensitive tissue at the back of the eye).
- In younger people, the lens is elastic and changes shape easily, allowing the eyes to focus clearly on both near and distant objects.
- As people reach their mid-40s, biochemical changes occur in the proteins within the lens, causing them to harden and lose elasticity. This loss of elasticity causes presbyopia, a type of vision problem that makes it more difficult to focus on close objects. This creates the need for reading glasses in almost everyone as they age.
- At this same stage there can be other changes in the lens that can affect the vision, but don't have much effect on the ability to read the eye chart. These changes include reduced ability to see in dim light, or sensitivity to glare. When considered together, these changes, including presbyopia, are called "dysfunctional lens syndrome".
- Cataracts develop when proteins in the lens clump together, forming cloudy (opaque) areas. The lens can also change color from transparent to a yellowish or brownish tint, which further worsens visual sharpness.
- Depending on how dense they are and where they are located, these cloudy areas can block the passage of light through the lens and interfere with the formation of images on the retina, causing vision to become cloudy.
- Age-related cataracts usually develop slowly over several years. With cataracts due to other causes, loss of vision may progress rapidly.
Some cataracts stop progressing after a certain point, but they never go away on their own. If extensive and progressive cataracts are left untreated they can cause blindness. In fact, cataracts are the leading cause of blindness among adults age 55 and older. Fortunately, cataracts can nearly always be successfully removed with surgery, greatly improving vision.
Cataracts can form in any of three parts of the lens and are named by their location:
- Nuclear sclerotic cataracts. Form in the nucleus (the center) of the lens. This is the most common type of cataract associated with the aging process. Nuclear cataracts increase nearsightedness and may initially improve close-up reading vision. As the cataract progresses, the lens color may darken, making it more difficult to distinguish colors and see clearly.
- Cortical cataracts. First form in the cortex (the outer edges of the lens) and then progress inwards to the center of the eye. They have a striped or spoke-like appearance. This type of cataracts can cause glare and also affect night vision and the ability to see contrast.
- Posterior subcapsular cataracts. Form toward the back of the capsule that surrounds the lens. They can cause glare or halos and tend to affect near vision more than distance vision.
Causes
Most cataracts are due to age, but there are other causes as well. Doctors categorize cataracts based on their cause:
- Age-related (cataracts due to the aging process)
- Secondary (cataracts caused by other medical conditions or treatments)
- Radiation (cataracts caused by exposure to ultraviolet or other radiation)
- Traumatic (cataracts caused by injury to the eye)
- Congenital (cataracts that appear at birth or early childhood caused by inherited disorders or infections that occurred during pregnancy)
Aging is the most common cause of cataracts. Cumulative effects of exposure to sunlight, irradiation, toxins, drugs, and disease cause the modification of proteins in the lens that makes them clump together. One of the causes of lens protein modifications is oxidative stress.
Oxidative stress is an imbalance between oxidants and antioxidants:
- Oxygen-free radicals (also called oxidants) are molecules produced by natural chemical processes in the body. Toxins, smoking, ultraviolet radiation, infections, and other factors can create reactions that produce excessive amounts of oxygen-free radicals.
- When oxidants are overproduced, these chemicals can be very harmful to cells throughout the body.
- Protective antioxidants, such as glutathione, help fight oxidants.
- Cataract formation is one of many damaging changes that can occur from overproduction of oxidants, possibly in combination with deficiencies of glutathione.
One theory is that in the aging eye, barriers develop that prevent glutathione and other protective antioxidants from reaching the nucleus in the lens, thus making it vulnerable to oxidation.
Secondary cataracts refer to cataracts that result from another medical condition or medical treatment. Causes of secondary cataracts include:
- Medications. Long-term use of oral corticosteroids (steroids) is a well-known cause of cataracts. It is unclear whether inhaled and nasal-spray steroids increase the risk for cataracts. Other types of medications can also increase the risk for cataract development.
- Medical Conditions. Medical conditions that increase the risk for cataracts include diabetes, high blood pressure, obesity, and skin conditions such as atopic dermatitis (a type of eczema). Medical conditions that require long-term use of oral steroids are associated with secondary cataracts.
- Eye Conditions and Eye Surgery. The inflammatory eye condition known as uveitis is strongly associated with cataracts. Glaucoma does not increase the risk for cataracts but certain types of surgery (trabeculectomy) and medications (miotics) used to treat glaucoma do increase cataract risk. Other types of eye surgery associated with cataract development are vitrectomy and peripheral iridectomy.
Cataracts can develop from overexposure to radiation, including sunlight. A common cause of radiation cataracts is the ionizing radiation used during treatment for head and neck cancer. Cataracts are also a side effect of total body radiation treatments, which are administered for certain cancers.
Traumatic cataracts are caused by blunt or penetrating injury to the eye. This type of cataract can develop immediately after the injury or many years later.
In rare cases, a baby is born with cataracts or develops them during infancy. Causes of congenital cataracts include:
- Genetic disorders (Down or Marfan syndrome)
- Prenatal infections (rubella or herpes simplex)
- Maternal abuse of alcohol or drugs during pregnancy
Risk Factors
Aging is the primary risk factor for cataracts, but other factors are also involved.
Nearly everyone who lives long enough will develop cataracts to some extent. Some people develop cataracts during their middle-aged years (40s and 50s), but these cataracts tend to be very small. It is after age 60 that cataracts are most likely to affect vision. Nearly one half of people age 75 and older have cataracts.
Women face a higher risk than men.
Cataracts tend to run in families.
In the United States, several prevalence studies have shown that cataracts are more likely to be a cause of vision impairment in blacks than in whites. This may be due to limited access to health care among non-white populations.
Certain medical conditions and treatments increase the risk for cataracts:
- Diabetes (type 1 or type 2) poses a very high risk for cataracts and the likelihood of developing them at a younger age. Cataract development is significantly related to high levels of blood sugar (hyperglycemia). (Cataract prevention is one of the many important benefits of controlling blood sugar.) Obesity, which is associated with diabetes type 2, and high blood pressure are also risk factors for cataracts.
- Long-term use of oral corticosteroids (commonly called steroids) increases the risk for cataracts. Medical conditions that use oral steroid medications for treatment include autoimmune diseases such as rheumatoid arthritis and systemic lupus erythematosus.
- Radiation therapy for head and neck cancer is a risk factor for cataracts.
- Eye injuries and certain types of eye surgeries (such as trabeculectomy for glaucoma) increase the risk for cataracts. Uveitis is an inflammatory eye condition that is a significant risk factor for cataracts.
- Nearsightedness (myopia) may be associated with increased risk for certain specific types of cataracts although it is uncertain whether it increases the general risk for age-related cataracts. Myopia does increase the risk for complications from cataract surgery.
Excessive exposure to ultraviolet B (UVB) radiation from sunlight increases the risk for cataracts. The risk may be highest among those who have significant sun exposure at a young age. People whose jobs expose them to sunlight for prolonged periods are also at increased risk.
Sunglasses or a wide-brimmed hat can help block the harmful effects of ultraviolet (UV) radiation. Protective sunglasses do not have to be expensive but it is important that they block 99% to 100% of UV light. Polarized, mirror-coated, or blue light-blocking lenses do not protect against UV radiation.
Smoking
Smoking a pack of cigarettes every day doubles the risk of developing cataracts. Smokers are at particular risk for cataracts located in the nuclear portion of the lens. Quitting smoking can help reduce the risk, although the risk will remain higher in former smokers than those who never smoked.
Alcohol
Chronic heavy drinkers are at high risk for a number of eye disorders, including cataracts.
Nutrition
Although it is not clear how much of a role nutrition plays in age-related cataracts, there is evidence that antioxidant-rich fruits and vegetables may offer some protection. The antioxidants most studied for cataract prevention are lutein and zeaxanthin, which are a type of antioxidants called carotenoids. Lutein and zeaxanthin are found in the lens.
Some research suggests that foods that contain these carotenoids, such as green leafy vegetables, may help slow the aging process in the eye and protect against cataracts. However, studies indicate that dietary supplements that contain lutein and zeaxanthin, or antioxidant vitamins, such as vitamin C or E, do not reduce the risks for cataract formation.
Antioxidants found in food, not supplements, appear to offer the best protection. Kale, collard greens, and spinach are the main food sources for lutein and zeaxanthin.
Symptoms
During the early stages, cataracts have little effect on vision. People who have small cataracts can often see well enough around the clouded areas to function normally. But as a cataract grows larger and increasingly clouds the lens, it can interfere greatly with daily activities such as reading and driving.
As a cataract progresses, symptoms may include:
- Cloudy, blurry, or dim, vision. You may feel as if you are seeing objects through a fog or veil. It can become difficult to see clearly even in brightly lit environments, and may be extremely difficult to see at night.
- Glare, halos, and sensitivity to bright lights. You may notice halos of light around streetlights or the headlights of oncoming cars, which can make it difficult or impossible to drive at night.
- Muted or faded colors. Images may take on a yellowish tint as color vibrancy diminishes.
- Reduced contrast. Reading may become difficult because of a reduced contrast between letters and their background.
- Double vision or "ghost" images in a single eye. A cataract can cause you to see multiple images or to see faint shadow copies of an image.
- Frequent change in corrective lenses. As the cataract grows, it can affect both near and far vision (and even cause temporary improvement.) You may find that you often need new prescriptions for eyeglasses or contact lenses.
- Symptoms may vary depending on the part of the lens that is affected. For example, posterior subcapsular cataracts, which cloud the center of the back of the lens, can make it difficult to read and to see in bright light when the pupil of the eye gets smaller. Cortical cataracts can worsen problems with glare. Nuclear cataracts, because of their brownish tint, typically cause problems seeing colors correctly, although this may not be detectable until the first eye has cataract surgery, causing the brownish tint in the un-operated eye to become obvious.
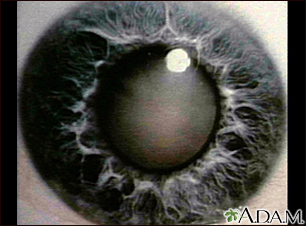
This photograph shows a cloudy white lens (cataract) seen through the pupil. Cataracts are a leading cause of decreased vision in older individuals, but children may have congenital cataracts. With new surgical techniques, the cataract can be removed, a new lens implanted, and the person can usually return home the same day.
Diagnosis
Either an ophthalmologist or an optometrist can examine people for cataracts, but only ophthalmologists are qualified to treat cataracts.
- An ophthalmologist is a medical doctor (M.D. or D.O.) who specializes in the medical and surgical care of the eye.
- An optometrist is a doctor of optometry (O.D.) who diagnoses eye diseases and prescribes corrective lenses but does not perform surgery.
The main tests used by an eye care professional to diagnose cataracts are:
- Visual acuity
- Ophthalmoscopy
- Tonometry
All of these tests are quick and painless.
Visual acuity tests evaluate how clearly a person can see. The Snellen eye chart is often used, with rows of letters decreasing in size:
- From a specified distance, usually 20 feet, a person reads the letters using one eye at a time.
- If a person can read down to the small letters on the line marked 20 feet, then vision is 20/20 (normal vision).
- If a person can read only down through the line marked 40 feet, vision is 20/40; that is, from 20 feet the person can read what someone with normal vision can read from 40 feet.
- If the large letters on the line marked 200 feet cannot be read with the better eye, even with glasses, the person is considered legally blind.
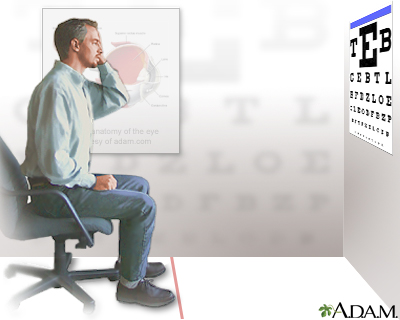
The visual acuity test can be performed in many different ways. It is a quick way to detect vision problems and is frequently used in schools or for mass screening.
Ophthalmoscopy is performed to examine the back part of the eye (fundus), which includes the retina, optic nerve, and blood vessels. This test can help detect cataracts as well as other eye diseases such as glaucoma. The eye doctor may give you eye drops before the test to dilate (widen) the pupils of your eyes.
There are several ways that ophthalmoscopy can be performed:
- Direct ophthalmoscopy. The eye doctor uses a handheld device (ophthalmoscope) to shine a beam of light through the pupil.
- Indirect ophthalmoscopy. The eye doctor wears a head lamp (like a miner's light) and a handheld lens to view the eye.
- Slit-lamp ophthalmoscopy. The doctor has you rest your chin and forehead on a support to keep the head steady, and then uses a special microscope and vertical beam of light to examine the eye.
Tonometry measures the pressure inside your eye. It is used to find out if glaucoma is contributing to your symptoms, although glaucoma rarely causes visual symptoms unless it is advanced. The clinician will first give you anesthetic drops to numb your eye. Next, a small device is gently pressed against your eye to measure intra-ocular (inside the eye) pressure. Eye pressure may also be evaluated in different ways such as with a hand-held electronic device or a gentle puff of air to indent the eye.
Other tests that may be used to diagnose cataracts or to determine if surgery is needed include:
- Contrast sensitivity. A chart similar to the Snellen chart is used to test contrast sensitivity. The chart has the same size letters, but in different contrasts with the background.
- Glare sensitivity. Glare sensitivity is tested by having the patient read a chart twice, with and without bright lights shining into the eyes.
- Potential acuity. Potential acuity evaluates the eye's acute vision center by testing macular function. It can help the ophthalmologist determine the expected improvement from cataract surgery.
- Endothelial cell count. The corneal endothelium, a layer of cells lining the inside of the cornea, is sensitive to normal surgical trauma and should be evaluated before any intraocular operation.
- People with other eye disorders may need other pre-operative tests.
Treatment
Surgery is the only cure for cataracts, but it is often not an emergency. Most cataracts cause no other health problems besides reducing a person's ability to see. Usually, there is no harm in reasonably delaying surgery, except for an increased risk of injury from falls or unsafe driving. Sometimes delaying surgery will cause a moderate (easy to perform surgery on) cataract to progress to an advanced (difficult to perform surgery on) cataract. The risks of surgical complications can be increased in advanced cataract. People usually have plenty of time to carefully consider options and discuss them with an ophthalmologist.
There is no constant rate at which cataracts progress:
- Some cataracts develop to a certain point and then stop, and may progress later.
- Even if a cataract does progress, it may be months or years before it interferes with vision. Your doctor may recommend "watchful waiting" and delaying surgery while monitoring your condition on an on-going basis.
- It is uncommon for people to need immediate cataract surgery.
The following measures may help manage early cataracts:
- Stronger eyeglasses or contact lenses
- Stronger indoor lighting
- Use of a magnifying glass during reading
Cataract removal is one of the most common types of eye surgery performed in the United States, especially for people over age 65. In the past, with older techniques, cataract surgery was not performed until the cataract had become well developed (ripe.) Newer techniques, however, have made it safer and even more efficient to operate in earlier stages. Cataract surgery improves vision in up to 95% of people and prevents millions of people from going blind. Femtosecond laser technology has also become a commonly utilized technology to complete part of the cataract surgery.
In general, after cataracts are diagnosed, the decision to remove them should be based on the person's own perception of vision difficulties and the effect of vision loss on normal activity or independent living. However, since progression is often gradual and subtle, it may not be apparent how they have affected vision and activities of daily life. Those considering cataract surgery should be made fully aware of all the potential risks and benefits of surgery.
You should ask the ophthalmologist the following questions before deciding to have cataract surgery:
- Is my cataract surgery an emergency?
- Are the cataracts the only cause of my poor vision?
- How much experience do you have with this procedure?
- Do I have other eye diseases that might complicate surgery or reduce my benefit?
- Do I have other health problems that might further complicate eye surgery?
- What type of lens will you implant?
- What type of procedure will you use?
- What are my chances of having poorer vision after surgery?
- How well should I ultimately be able to see out of the operated eye?
- How long will it take to heal?
- What precautions should I take during the healing process?
- How long will it take to achieve my best eyesight?
- Will I have to wear glasses or contact lenses after surgery?
- When will I get my final eyeglass prescription?
- How soon after surgery will I be able to see well enough to go back to work? Drive a car? Return to full activity?
If you have further questions or doubts about the procedure, you may want to get a second opinion from another ophthalmologist.
Cataracts in the Second Eye
If a person has a cataract in a second eye, the issues for decision-making are the same as for the first eye. In general, surgery for a second cataract is usually performed at least 1 to 2 weeks after surgery for the first eye. Although uncommon, in some circumstances surgery may be performed on both eyes at the same time.
Cataracts and Glaucoma
There are various approaches to treating people who have both cataracts and glaucoma. Your doctor will recommend an approach based on your individual condition. Some options include:
- For people who have mild glaucoma, the doctor may recommend performing only cataract surgery and controlling the glaucoma with medication.
- For people who have moderate to severe glaucoma, the traditional approach has been combination cataract-glaucoma surgery (phacotrabeculectomy.) This combination surgery involves performing both trabeculectomy (glaucoma filtration surgery) and phacoemulsification (cataract extraction).
- Newer techniques and devices are being developed for MIGS (minimally invasive glaucoma surgery or micro-invasive glaucoma surgery), most of which can be combined with cataract surgery. They have the advantages of generally being safer and more effective than trabeculectomy. For example, the iStent is a tiny tube that is implanted in the eye during cataract surgery. The stent helps improve the outflow of aqueous humor which is a fluid, and thereby lower intraocular pressure (IOP) in the eye.
Infants
Treatment of infants first depends on whether one or both eyes are affected:
- For infants born with cataracts in one eye, the American Academy of Ophthalmology recommends surgery as soon as possible, by age 4 months or ideally even earlier. The procedure is followed by contact lens correction and patching of the unaffected eye. Although this approach is successful in many cases, some children still become blind in the affected eye. There is also a high risk for glaucoma after surgery.
- For infants with cataracts in both eyes, surgery is not always an option. Sometimes surgery may be performed sequentially, with the second eye operated on a few days after the first. Phacoemulsification appears to pose a much higher risk for secondary cataracts than standard lens removal.
Toddlers and Older Children
Intraocular lens replacement is now standard treatment for children age 2 years and older.
Surgery
Cataract surgery is usually done as an outpatient procedure under local anesthesia and takes less than an hour. Preoperative preparations may include:
- A general physical examination for people with medical problems, such as diabetes. Diabetes can cause damage to the blood vessels of the retina, a condition called diabetic retinopathy. If you have diabetes, discuss with your doctor how your blood sugar level may affect the surgery.
- A review of all your medications. In particular, men who take tamsulosin (Flomax), or similar drugs for prostate problems, require special surgical techniques to prevent complications.
- A painless test to measure the length of the eye and determine the type of replacement lens that will be needed after the operation.
- Topical antibiotics (for example, ofloxacin or ciprofloxacin), which may be applied for a day or two before surgery to protect against postoperative infection. Topical non-steroidal anti-inflammatory drugs (NSAIDs) such as ketorolac may also be used before surgery.
All cataract procedures involve removal of the lens (cataract extraction) and replacing it with an artificial lens called intraocular lens (IOL). Cataract extraction is performed by one of three procedures:
- Phacoemulsification
- Extracapsular cataract extraction
- Intracapsular cataract extraction -- rarely used today
Anesthesia for Cataract Surgery
There are three methods of providing anesthesia for cataract surgery. Depending on the surgery and the patient, one or more of these techniques may be used:
- Topical anesthesia
- Local anesthesia
- General anesthesia
Topical anesthesia involves topical drops that numb the surface of the eye, and a tiny amount of anesthetic that is injected directly into the eye at the beginning of the actual surgery. Nothing specifically blocks the nerves of the muscles that move the eye. Sedation in the form of an injection through a vein or occasionally as a pill, will help the patient hold the eye still.
In local anesthesia, a sedative injection through a vein is given, followed by injections of anesthetic around the eye to numb the eye and block the nerves to the eye muscles.
General anesthesia is the method of choice for babies, children, and adults who are not able to cooperate.
Phacoemulsification
Phacoemulsification (phaco means lens; emulsification means to liquefy) is the most common cataract removal method in the United States.
The procedure generally involves the following:
- The surgeon makes a small incision at the edge of the cornea.
- The phacoemulsification probe is inserted into the eye. This probe has a hollow vibrating needle attached to a vacuum source. The needle is surrounded by a silicone sleeve.
- Cataract fragments are drawn to the tip of the needle where ultrasonic vibrations break them up so they can be sucked out through the core of the needle.
- To keep the eye inflated during this process, irrigation fluid flows around the needle under the silicone sleeve and back into the eye.
- An artificial intraocular lens is implanted in place of the natural lens.
Most phacoemulsification procedures take about 15 minutes, and the patient is usually out of the operating room in under an hour. There is little discomfort afterward, and complete visual recovery usually occurs within 1 to 5 days.
Phacoemulsification is sometimes combined with glaucoma surgical procedures, for people who have both glaucoma and cataracts.
Extracapsular Cataract Extraction
Extracapsular cataract extraction, the precursor to phacoemulsification, is now generally used only in people who have an extremely hard lens.
The procedure generally involves the following:
- The surgeon makes a larger incision at the edge of the cornea.
- The hard center (nucleus) of the lens is loosened from the rest of the cataract.
- The nucleus is removed in one piece through the larger incision.
- The incision is closed with stitches.
- An irrigation/aspiration probe (similar to a phacoemulsification probe but without the ultrasound) is used to remove the remaining, softer parts (cortex) of the cataract.
- An artificial intraocular lens is implanted in place of the natural lens.
Laser Cataract Surgery
Newer technologies have been developed so that the incisions used in cataract surgery can be made with a femtosecond laser rather than a blade. (The femtosecond laser was originally developed to make the flap in LASIK surgery. It has since been modified to be useful in cataract surgery.) Femtosecond laser also performs a crucial step of cataract surgery called capsulorhexis (making a circular opening of the front membrane of the cataract.) The laser can also soften the lens nucleus so that phacoemulsification will be easier. It still remains to be seen whether laser cataract surgery presents clear advantages over more conventional methods.
Regardless of which technique is used to remove the cataract, a lens implant (IOL) is almost always inserted to correct the optics of the eye, which now has no natural lens.
With the clouded lens removed, the eye cannot focus a sharp image on the retina and is functionally blind at all distances. A replacement lens is therefore needed.
Intraocular Lenses (IOLs). An artificial lens, known as an intraocular lens (IOL), is usually inserted immediately after the cataract is extracted. Most IOLs are made out of acrylic, although other materials, such as silicon, are also used.
IOLs are designed to improve specific aspects of vision. In the United States, there are currently 4 choices:
- Monofocal IOLs. These have been used since the 1980's. They can correct either distance or near vision, but not both. Glasses will be needed for the range that is not corrected by the IOL, as well as astigmatism; for example, if the eye can see at distance with the IOL, then glasses will be needed for reading.
- Multifocal IOLs. These have been available since about 2004 and can correct both nearsightedness and farsightedness. However, contrast may be slightly reduced, and some patients may experience mild glare and halos, particularly at night.
- Toric IOLs. These were FDA-approved in 1998. These lenses are designed to correct pre-existing astigmatism, as well as nearsightedness and farsightedness in patients having cataract surgery.
- Trifocal IOLs. The first trifocal IOL has been approved by the FDA in 2019. It can correct near, intermediate, and distance vision and is available in spherical and toric designs.
The patient and the doctor must choose the IOL based on specific visual needs. Many people also need eyeglasses after cataract surgery for reading or to correct astigmatism.
Cataract surgery is one of the safest of all surgical procedures. Most complications are not serious. They can include:
- Swelling and inflammation. A small amount of inflammation in the area where the cataract surgery took place is common for a day or two after the surgery. Swelling and inflammation can occur elsewhere in the eye; although the risk is about 1%, this complication can be particularly harmful for people with a prior history of uveitis (chronic inflammation in the eye, which can be due to various medical conditions).
- Retinal detachment. In rare cases, the retina at the rear of the eye can become detached from the inside of the eye. If this happens, it needs to be treated promptly.
- Infection. This is very rare (0.2%) but may be serious if it does develop.
- Bleeding inside the eye.
- Posterior capsular opacification. This condition is also known as a secondary cataract that involves clouding of the lens capsule, and is one of the more common complications of cataract surgery. This can be treated with an in office laser procedure.
Glaucoma
This is suspected when the eye pressure is elevated. If this occurs after cataract surgery, it is usually one of three forms:
- Rapid onset, usually seen on the first day after surgery, with high pressures; this is a response to one of the agents used during cataract surgery; treatment rapidly lowers the pressure and it is usually completely resolved within a week.
- Elevated pressure that results from the corticosteroid drops used during the post-operative period; this occurs in "steroid responders" and goes away when the drops are stopped.
- A more gradual increase in pressure that occurs over weeks to months; this is more likely to develop into true glaucoma, but is rare.
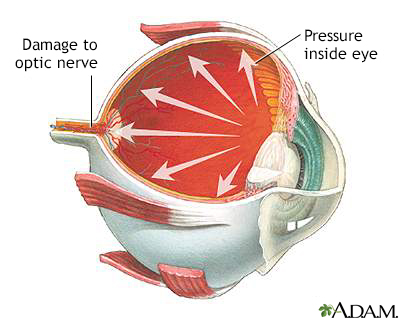
Glaucoma is a disorder of the optic nerve that is usually marked by increased fluid pressure inside the eye. The increased pressure causes compression of the retina and the optic nerve which can eventually lead to nerve damage. Without treatment, glaucoma can cause partial vision loss, with blindness as a possible eventual outcome.
Factors that Increase Risk for Complications
The risks of complications are greater if you have:
- Other eye diseases.
- Diabetes. Cataract extraction can pose a high risk for the development or worsening of retinopathy, a known eye complication of diabetes.
- Taken tamsulosin (Flomax) or other alpha-1 blocker drugs. Tamsulosin is a muscle relaxant prescribed for treatment of several urinary conditions, including benign prostatic hyperplasia (BPH.) Tamsulosin may cause intraoperative floppy iris syndrome (IFIS), a loss of muscle tone in the iris that can cause complications during eye surgery. Problems have been reported both for people who were taking the drug at the time of surgery as well as those who had stopped taking the drug for several weeks or months before surgery. Men who have taken tamsulosin or similar drugs should inform their eye surgeon. The surgeon may need to use different techniques to minimize the risk of complications from IFIS.
Preventing Infection and Reducing Swelling
The ophthalmologist may prescribe the following medications after surgery:
- A topical antibiotic for protection against infection.
- Corticosteroid eye drops or ointments to reduce swelling, such as prednisolone. They may pose a risk for increased pressure in the eye.
- Nonsteroidal anti-inflammatory drugs (NSAIDs), such as diclofenac, ketorolac, naproxen, and voltaren. NSAIDs also reduce swelling and do not have the same risks (increased eye pressure) as steroids. Newer NSAIDs approved to treat pain and swelling after cataract surgery include bromfenac (Prolensa, Xibrom) and nepafenac (Ilevro, Nevanac).
- Some ophthalmologists may inject antibiotics and corticosteroids into the eye at the end of the surgery, reducing the number of medications that must be used during the post-operative period.
Returning Home and Follow-up Visits:
- You will probably leave the surgical site within about an hour after surgery. Cataract surgery almost never requires an overnight hospital stay.
- You will need someone to drive you home and stay with you for a few days until your vision improves.
- You will be examined a day or two after surgery and then during the following month. Additional visits occur as necessary.
- For routine cataract surgery, vision has usually recovered by day 5, often sooner. Rarely the vision may remain blurry for up to 6 weeks. If complications occur during surgery, vision recovery may take longer than that.
- When your doctor decides the condition has stabilized, you will receive a final prescription for glasses or contacts.
Protecting the Eye
Postoperative protection of the eye typically involves the following actions:
- The ophthalmologist usually tapes a bandage and a rigid eye shield over the eye at the end of surgery.
- Most surgeons don't require any bandages after the first post-operative visit except to wear just the rigid eye shield at night for the first week.
Other postoperative advice includes:
- Avoid rubbing the eye.
- Use dark glasses whenever in bright sunlight.
- Avoid swimming and exposure to dust and wind.
- Do not bend over unnecessarily for at least one week following surgery.
- Refrain from jumping, running, heavy lifting, and any other strenuous exercise for a few weeks after surgery.
About 15% of people who have cataract surgery develop a secondary or "after-cataract" called posterior capsular opacification. Posterior capsular opacification is a clouding of the lens capsule that was intentionally left behind, (it is used to hold the IOL in place) when the original cataract was removed. It generally occurs because some cells of the natural lens remain after surgery and can regrow onto the capsule.
The standard treatment for posterior capsular opacification is a type of laser surgery known as a YAG capsulotomy. (Capsulotomy means making an opening in the capsule, and YAG is an abbreviation of yttrium aluminum garnet, the laser most often used for this procedure.) This is an outpatient procedure that involves no incision and can help improve vision and reduce glare.
YAG capsulotomy involves the following:
- The Yag laser has a chinrest and forehead bar for the patient, similar to what is used for a slit lamp exam. Some surgeons use a contact lens to help aim the laser, but if not, nothing will touch the eye.
- There is no pain and the procedure is usually complete within a minute or two.
- After the procedure, the patient may remain in the doctor's office for an hour to make sure that pressure in the eye is not elevated.
- The doctor will usually prescribe anti-inflammatory eyedrops for the person to take at home.
- Most people will find that their vision improves within a day.
- An eye examination for any complications should follow within 2 weeks.
Complications
YAG laser capsulotomy is generally a safe procedure. Serious complications are rare, but can include retinal detachment.
Resources
- American Academy of Ophthalmology -- www.aao.org
- National Eye Institute -- www.nei.nih.gov
- Eye Smart -- www.aao.org/eye-health
References
Allen D. Phacoemulsification. In: Yanoff M, Duker JS, eds. Ophthalmology. 5th ed. Philadelphia, PA: Elsevier; 2019:chap 5.9.
Allman KG. Anesthesia for cataract surgery. In: Yanoff M, Duker JS, eds. Ophthalmology. 5th ed. Philadelphia, PA: Elsevier; 2019:chap 5.8.
Chang JR, Koo E, Agrón E, et al; Age-Related Eye Disease Study Group. Risk factors associated with incident cataracts and cataract surgery in the Age-related Eye Disease Study (AREDS): AREDS report number 32. Ophthalmology. 2011;118(11):2113-2119. PMID: 21684602 www.ncbi.nlm.nih.gov/pubmed/21684602.
Chiu CS. 2013 update on the management of posterior capsular rupture during cataract surgery. Curr Opin Ophthalmol. 2014;25(1):26-34. PMID: 24310374 www.ncbi.nlm.nih.gov/pubmed/24310374.
De Silva SR, Evans JR, Kirthi V, Ziaei M, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev. 2016;12:CD003169. PMID: 27943250 www.ncbi.nlm.nih.gov/pubmed/27943250.
Howes FW. Manual cataract extraction. In: Yanoff M, Duker JS, eds. Ophthalmology. 5th ed. Philadelphia, PA: Elsevier; 2019:chap 5.12.
Howes FW. Patient workup for cataract surgery. In: Yanoff M, Duker JS, eds. Ophthalmology. 5th ed. Philadelphia, PA: Elsevier; 2019:chap 5.4.
Kohnen T, Wang L, Friedman NJ, Koch DD. Complications of cataract surgery. In: Yanoff M, Duker JS, eds. Ophthalmology. 5th ed. Philadelphia, PA: Elsevier; 2019:chap 5.16.
Lambert SR, Aakalu VK, Hutchinson AK, et al. Intraocular lens implantation during early childhood: a report by the American Academy of Ophthalmology. Ophthalmology. 2019;126(10):1454-1461. PMID: 31230794 www.ncbi.nlm.nih.gov/pubmed/31230794.
Lim BX1, Lim CH, Lim DK, et al. Prophylactic non-steroidal anti-inflammatory drugs for the prevention of macular oedema after cataract surgery. Cochrane Database Syst Rev. 2016;11:CD006683. PMID: 27801522 www.ncbi.nlm.nih.gov/pubmed/27801522.
Liu YC, Wilkins M, Kim T, Malyugin B, Mehta JS. Cataracts. Lancet. 2017;390(10094):600-612. PMID: 28242111 www.ncbi.nlm.nih.gov/pubmed/28242111.
Lundström M. Outcomes of cataract surgery. In: Yanoff M, Duker JS, eds. Ophthalmology. 5th ed. Philadelphia, PA: Elsevier; 2019:chap 5.18.
National Eye Institute website. Cataract data and statistics. www.nei.nih.gov/learn-about-eye-health/resources-for-health-educators/eye-health-data-and-statistics/cataract-data-and-statistics. Updated July 2019; Accessed November 11, 2019.
Olson RJ, Braga-Mele R, Chen SH, et al. Cataract in the adult eye preferred practice pattern. Ophthalmology. 2017;124(2):P1-P119. PMID: 27745902 www.ncbi.nlm.nih.gov/pubmed/27745902.
Packer M. Small incision and femtosecond laser cataract surgery. In: Yanoff M, Duker JS, eds. Ophthalmology. 5th ed. Philadelphia, PA: Elsevier; 2019:chap 5.11.
Rautiainen S, Lindblad BE, Morgenstern R, Wolk A. Total antioxidant capacity of the diet and risk of age-related cataract: a population-based prospective cohort of women. JAMA Ophthalmol. 2014;132(3):247-252. PMID: 24370844 www.ncbi.nlm.nih.gov/pubmed/24370844.
Salmon JF. Lens. In: Salmon JF, ed. Kanski's Clinical Ophthalmology. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 10.
Wevill M. Epidemiology, pathophysiology, causes, morphology, and visual effects of cataract. In: Yanoff M, Duker JS, eds. Ophthalmology. 5th ed. Philadelphia, PA: Elsevier; 2019:chap 5.3.
Zhang ML, Hirunyachote P, Jampel H. Combined surgery versus cataract surgery alone for eyes with cataract and glaucoma. Cochrane Database Syst Rev. 2015;(7):CD008671. PMID: 26171900 www.ncbi.nlm.nih.gov/pubmed/26171900.
Reviewed By: Audrey Tai, DO, MS, Assistant Clinical Professor (Voluntary), University of California - Irvine, Irvine, CA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.






